By Dr Fiona McMillan
Diffuse Large B-Cell Lymphoma (DLBCL) is the sixth most common form of cancer worldwide. It’s a blood cancer that arises from white blood cells called B-cells, which normally play an important role in enabling your immune system to identify and attack potentially harmful viruses and bacteria. Your body makes millions of B-cells each day, and sometimes one of these cells becomes malignant. The cause of this remains unknown.
Every year there are up to 2000 new cases of DLBCL in Australia alone. While the disease occurs most often in people over 50, it can strike at any age. Moreover, it can be fast growing and aggressive, so early diagnosis is vital, as is swift treatment. Fortunately, the majority of DLBCL cases respond very well to the current frontline treatment, called R-CHOP, which is a combination of chemotherapy and immunotherapy. About 70% of patients are cured by this approach. However, a subset of patients simply don’t respond to R-CHOP. For these people, the prognosis is poor. With the advance of new immunotherapy treatments that have shown benefits in other cancers, it would be ideal to be able to figure out which patients are unlikely to respond to standard treatment and instead allow them to trial experimental treatments as soon as possible. R-CHOP treatment lasts around four months; such a delay can be life-threatening. Moreover, the new immunotherapies are extremely expensive, and come with their own range of side-effects. As such, clinicians need good cause to choose this course of action for a patient over standard treatment. To make this decision, we need to be able to identify at an early stage which patients will respond to R-CHOP and are likely to be cured by it, and which patients won’t.
Professor Maher Gandhi is the Leukaemia Foundation Queensland Chair in Blood Cancer Research at the University of Queensland Diamantina Institute. He explains that the challenges in predicting patient outcomes to treatment arise because there is still a lot we don’t know about DLBCL and how it interacts with the immune system.
“The problem is that we are not capturing the complexity of lymphoma adequately with our current tests, and that means we fail to accurately predict patient outcome,” says Professor Gandhi. “And the reason we’re failing is because we’re focusing on only two aspects of lymphoma and there are three.”
So far researchers and clinicians have concentrated on the clinical presentation of the patient, Professor Gandhi explains, and on the biology of the cancer cell itself, particularly the aggressiveness of malignant cells.
“What we haven’t focused on is the tumour microenvironment,” he says. “And that’s what we set out to do.”
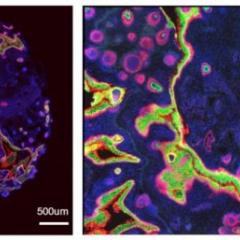
The tumour microenvironment is the local area immediately surrounding the tumour, this is where it interacts with blood vessels, connective tissue, and the patient’s immune system. To survive, the tumour must access nutrients via the microenvironment as well as shield itself from harmful immune cells. After all, the immune system has evolved to not only eliminate foreign threats, such as pathogens, but to also destroy the body’s own cells when they malfunction. Therefore, a critical step in the progression of a tumour is its ability to alter the microenvironment so that the normal behaviour of immune cells is disrupted.
We now know that tumour cells can recruit a patient’s immune cells to protect it and help it grow. They do this by turning some of the patient’s immune cells against the rest. These particular cells are part of the normal checks and balances that prevent the immune system from running out of control; their job to calm down attack-ready immune cells when needed. By sending the right signals, tumour cells trick these cells into to subduing tumour-killing immune cells.
Moreover, recent studies in solid tumours reveal a remarkable, almost counterintuitive effect: the ability to turn the immune system against itself is not weakened in response to treatment, instead it gets stronger. If we were to see treatment as an offensive strike, then the tumour ramps up its defence in direct response, recruiting more immune cells and making them ‘tumour-friendly’. How well a tumour does this can determine the outcome for the patient.
Professor Gandhi wondered if this was also happening in DLBCL and if so, whether this effect is responsible for why some people respond well to R-CHOP and some don’t. He reasoned that if this was indeed the case, then there may be a way to predict patient outcomes just by looking at a sample of immune cells in the tumour microenvironment.
The first step was to determine whether DLBCL tumours also ramp up their ability to cause immune cell betrayal in response to treatment in the way that solid tumours do. Blood cancers differ significantly from solid tumours in their physical structure, and in their microenvironment. To use a rough analogy, a compact solid tumour in its microenvironment is like a hand in a glove, whereas the tumour cells of blood cancers like DLBCL are spread out, more like a mesh, with the microenvironment flowing amongst and around them.
Gandhi and his colleagues worked closely with biostatisticians and large patient groups both in Australia and around the world. They analysed samples of patient tumours and determined which immune cells were in the microenvironment by identifying which genes were present. Specifically, they looked for genes associated with anti-tumour immune cells as well as genes commonly found in immune cells that turn ‘tumour-friendly’. These are the genes responsible for quelling the tumour-killing immune cells.
The researchers discovered that DLBCL tumours do indeed ramp up their defence in response to treatment, turning more of the patient’s immune cells into tumour-friendly cells. The research team next looked at whether the proportion of tumour-friendly immune cells to anti-tumour immune cells would indicate how well the patient ultimately responded to treatment. By analysing the relative numbers of each immune cell type before treatment begins and then monitoring patient outcomes, they discovered that there was a direct link. Moreover, this could be quantified in a straightforward formula: patients with a high ratio of anti-tumour to pro-tumour immune cells have a greater than 90% chance of being cured by standard treatment (R-CHOP); patients with a low ratio are unlikely to benefit from standard treatment. The findings are published this week in the journal Lancet Haematology.
Professor Gandhi believes that this approach will now provide clinicians with a valuable tool that will help them identify who should continue standard treatment and who should be eligible for new clinical trials. His next goal is to determine whether this approach could be used in a similar manner to predict whether a patient is likely to benefit from the new wave of drugs targeting PD-1 and PD-L1, which are now major targets in anti-cancer therapies. Professor Gandhi is optimistic that collaborations such as the current one will continue to yield vital information about the intricate dynamics between cancer, the immune system, and treatments.
“Work like this demonstrates what can be achieved if clinicians, scientists and statisticians collaborate,” he says. “What you need is clever ideas, well designed studies and everyone working together. If you do that you can truly come up with answers that are as good as what anyone can come up with anywhere in the world.”
Media: Professor Maher Gandhi, m.gandhi@uq.edu.au, +61 7 3443 8026; Kate Templeman, k.templeman@uq.edu.au +61 7 3443 7027, +61 (0)409 916 801.