University of Queensland researchers have contributed to the development of a new approach to detecting coeliac disease, revealing the immune disorder is far more common than previously recognised.
In a study of more than 2500 Victorians, researchers combined measuring the immune response to gluten with an assessment of specific genetic risk markers, and found more than 50 per cent of Australians had genetic risk factors for developing coeliac disease.
“Coeliac disease is a common condition which is often hard to diagnose or exclude using standard tests. This is a great example of a condition where genetic tests offer substantial advantages for screening over what is currently available,” said Professor Matt Brown, Director of The University of Queensland Diamantina Institute.
Previously, it has been understood that coeliac disease affected up to one in 100 people. However new tests indicate that far more people are susceptible, with up to one in 60 Australian women and one in 80 Australian men affected.
The disease is caused by an inappropriate immune response to dietary gluten, found in wheat, rye, barley and oats.
It can cause a wide range of complaints from chronic tiredness, iron deficiency, osteoporosis, itchy rash and headaches to various digestive symptoms.
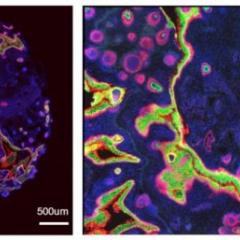
Coeliac disease damages the lining of the small intestine and can lead to significant medical complications such as autoimmune disease, infertility, liver failure and cancer.
The disease usually develops in childhood and is life-long, but early diagnosis and treatment can reduce the risk of adverse health complications.
Associate Professor Emma Duncan and Professor Matt Brown from The UQ Diamantina Institute, based at Translational Research Institute in Brisbane, have been in collaboration with researchers from Walter and Eliza Hall Institute, US biotechnology company ImmusanT, and researchers from Barwon Health, Deakin University and Healthscope Pathology, to develop and trial the new diagnostic approach.
Associate Professor Duncan said the genetic testing offered new hope for patients at risk of the disease.
“By testing just five genetic markers, potentially at a cost of a few cents each, we are able to determine who is at genetic risk of coeliac disease and conversely, who is not at risk, and therefore does not need further costly investigations such as endoscopy,” she said.
“This study represents a major improvement in our ability to work out which patients might benefit from more formal investigation.”
Walter and Eliza Hall Institute immunology department’s Dr Jason Tye-Din said the new approach of combining the genetic test with a panel of antibody tests would increase the accuracy of testing, decrease overall medical costs by reducing invasive diagnostic tests and avoid medically unnecessary use of a gluten-free diet.
“Currently, bowel biopsies are recommended for anybody with positive antibody tests,” he said.
“In this study the inclusion of a simple genetic test helped identify a substantial number of people whose antibody tests were falsely positive and who did not actually require a bowel biopsy to test for the possibility of coeliac disease.”
It is not yet known why the disease develops in only some people with genetic risk factors.
Dr Tye-Din said the findings were surprising and shed new light on the medical burden of coeliac disease in Australia.
“Accurate and timely diagnosis is important for the health of patients with coeliac disease. Making a diagnosis based on a blood test alone or commencing a gluten-free diet without a confirmatory bowel biopsy is inappropriate and can impose an unnecessary and lifelong treatment.
“Although small bowel biopsy is needed to confirm coeliac disease, it is costly and invasive. Reducing unnecessary procedures is better for patients, eliminating an invasive test, and better for the economy by reducing healthcare costs,” Dr Tye-Din said.
“This study provides a strategy to improve the diagnosis of coeliac disease in the community by combining the benefits of antibody and genetic testing.”
The research was funded by INOVA Diagnostics Inc, Nexpep Pty. Ltd, the NHMRC, the Victorian Health Promotion Foundation, the Geelong Region Medical Research Foundation and the Victorian government.
The research is published online in the journal BMC Medicine.