 Patients’ genes could unlock urgently needed new treatments for severe sepsis, which kills three and a half times as many Australians as the road toll.
Patients’ genes could unlock urgently needed new treatments for severe sepsis, which kills three and a half times as many Australians as the road toll.
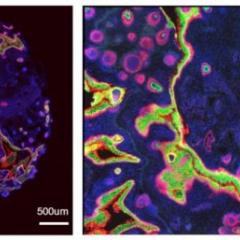
Researchers from The University of QueenslandDiamantina Institute and the George Institute for Global Health, Sydney, are investigating whether genetic variation between critically-ill patients contributes to their susceptibility to bacterial infection, the severity of their disease and their response to treatment.
Researcher Professor David Evans said researchers would analyse up to 1000 blood samples, creating a world-leading genomics resource to help develop new treatments for severe sepsis, including the possibility of personalised therapies.
“Severe sepsis remains a major cause of mortality and disability worldwide and we are working closely with an extensive network of clinical collaborators on this project,” Professor Evans said.
Samples will be collected from patients from 25 sites in Australia and New Zealand and will be analysed at the UQ Diamantina Institute.
In Australia there are more than 15,000 new cases of severe sepsis in the adult population each year, and approximately one in three adults admitted to hospital with the condition die within 28 days.
“The cause of death is most commonly due to multiple-organ failure,” Professor Evans said.
“By undertaking this study we hope to develop a model to predict 90 day mortality in sepsis patients, and determine which patients are likely to respond to a particular treatment.”
The study is running alongside a major randomised clinical trial of hydrocortisone therapy for severe sepsis patients.
The clinical trial, known as ‘ADRENAL’ is being led by intensive care specialist at the Wesley and Princess Alexandra Hospitals, Professor Bala Venkatesh.
Professor Venkatesh said there have previously been more than 70 research trials in the past two decades into new treatments for sepsis but the results have been disappointing.
“Two major trials have produced conflicting results, so there is now no consensus as to the use of hydrocortisone and there is a strong view this discrepancy reflects individual differences.
“It may be that corticosteroids would benefit some patients but could harm others, and the study led by Professor Evans could determine who will respond based on their genomic profile.”
Sample collection for the genome trial will continue into next year, with results expected in 2018.
Media: Professor David Evans d.evans1@uq.edu.au, +61 7 3443 7051. Kim Lyell, Faculty of Medicine and Biomedical Sciences, k.lyell@uq.edu.au, +61 7 33465214, 0427 530647.