Researchers at The University of Queensland Diamantina Institute are developing a new technology derived from turmeric that could provide hope for patients with type 2 diabetes.
In Australia, type 2 diabetes affects about 3.5% of the population and usually occurs in adults over the age of 45. It is primarily caused by lifestyle factors and is associated with obesity, hypertension and elevated cholesterol.
Insulin is a hormone produced by the pancreas which moves sugar from the food we eat into the body's cells. Patients with type 2 diabetes either cannot produce enough insulin or have a condition called ‘insulin resistance’, where the insulin they do produce is not used properly.
It is now known that insulin resistance arises due to misguided inflammation signals from the immune system. The immune cells that reside both in adipose (‘fat’) tissue and in the liver appear to be the major culprits: they release pro-inflammatory compounds that disrupt the way the body handles insulin.
Dr Brendan O’Sullivan, a Senior Research Officer at UQDI, and his team wanted to know precisely which immune cells in these tissues cause insulin resistance and whether this could be off-set by treating them with curcumin, the yellow ingredient derived from the spice turmeric.
“Curcumin, which is the yellow compound that you see in curries, has been used as a herbal remedy for diabetes for centuries,” explains Dr O’Sullivan. We now know that curcumin acts as a specific blocker of the inflammatory signals that arise in diabetes.
While curcumin can be consumed at high levels, the amount of bioactive curcumin within the blood is very low and is delivered to the entire body, rather than as a concentrated dose where it’s really needed.
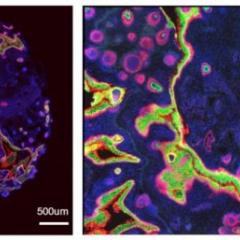
“By encapsulating curcumin in microscopic lipid droplets, they can be delivered to the liver and adipose tissue to prevent the production of diabetes-inducing inflammatory compounds,” he said.
These droplets, called ‘curcusomes’, were found to improve diabetes in mice by lowering levels of inflammatory compounds and subsequently reducing insulin resistance.
Moreover, the researchers were also able to precisely determine which immune cells triggered insulin resistance in the first place: a cell type called Tip-DCs in the liver and adipose tissue macrophages (ATMs) in fat tissue. This vital information expands our knowledge about how diabetes arises.
O’Sullivan’s team is now optimising the curcusome technology into a drug to prevent liver inflammation in obesity, a common precursor to diabetes.
If successful, the treatment could be combined with existing anti-diabetic drugs to reduce complications associated with diabetes in patients. Curcusomes may also prove effective in the treatment of other conditions such as cardiovascular disease, rheumatoid arthritis, and certain forms of liver disease.
Dr O'Sullivan received a Smart State Fellowship from the State Government and funding from Arthritis QLD to explore potential diabetes treatments.
Results from this study were recently published in Diabetes Journal.