By Dr Fiona McMillan
Every year in Australia, more than 4000 people are diagnosed with Head and Neck Squamous Cell Carcinoma (HNSCC). In more than half of these patients, the disease is already advanced and their prognosis is poor.
A known biological hallmark of HNSCC cells is that they produce unusually high levels of a protein called EGFR. This knowledge led to the development of an antibody designed to bind to and inactivate EGFR. The approach improved progression free survival, but only in a small proportion of HNSCC patients. It was not clear why.
A cross-discipline collaboration between two researchers at the University of Queensland Diamantina Institute is shedding new light on how this treatment works and their research is revealing new ways to substantially improve patient responses.
Dr Fiona Simpson, a cancer biology researcher at UQDI studied tumours from patients who respond well to the antibody and found that while it does indeed disrupt EGFR’s function, this only accounts for part of the therapeutic effect. Something else is going on.
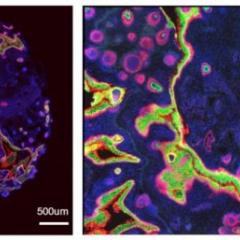
To find out, Simpson teamed up with Dr James Wells, a researcher in the immunology program at UQDI. Together they set up a series of assays that revealed the antibody’s other role: it triggers an immune reaction.
Normally, cancer cells send out signals that help them evade detection by the immune system, explains Wells. “But here, the antibody is acting as a bridge between the immune cells and the tumour cells.”
Simpson agrees. “This means that one of the ways that the therapy kills the tumour cells is by using an immune system response to the tumour,” she says.
Simpson and Wells then turned their attention to the mystery of why many HNSCC patients don’t respond well to the antibody. Simpson, who is an expert in cell trafficking, was able to determine that even though most HNSCC cells produce high levels of EGFR, the location of that EGFR is not the same in all patients.
She discovered that it’s a matter of access. In patients who respond well to the treatment, their cancer cells have EGFR on the cell surface where the antibody can easily bind to it. Immune cells can then see the antibody and trigger an immune response. Unfortunately for patients who don’t respond well, their cancer cells keep EGFR inside the cell where it can’t be reached by the antibody. And for many HNSCC patients, this seems to be the case.
Simpson is developing a test that will help doctors know ahead of time which patients will benefit from the treatment and which patients will not. But Simpson and Wells don’t want to stop there.
They are investigating ways to treat cancer cells with small molecules that help trap the EGFR on the cell surface, making it an easy target.
The assays they have set up allow them to see precisely which cells are dying when they test new compounds, because they want to kill tumour cells without damaging the immune system. So far the results are promising. The next step is to test the compounds in pre-clinical models of HNSCC and if successful, progress to human clinical trials.
Simpson and Wells believe the set up of the UQ Diamantina Institute played an important role in their collaboration by bringing together immunology and cancer programs in the same place and in the context of a strong clinical network.
“This is a really good way to do cross-field research,” says Simpson. “Most cancer research is moving toward developing immunotherapies, so these kinds of collaborations are essential to future success.”
Media: Kate Templeman, +61 7 3443 7027 or 0409 916 801, k.templeman@uq.edu.au