University of Queensland (UQ) researchers based at TRI are unlocking the secrets of melanoma cells to identify potential new drug targets and personalised treatment regimens for patients with the skin cancer, melanoma.
Collaborating with Queensland University of Technology (QUT) mathematicians including Professor Matthew Simpson, Professor Haass and his team recently debunked the longstanding ‘grow-or-go’ theory that melanoma cells only have enough energy to either proliferate (grow) or metastasize (go). Using both laboratory studies and mathematical modelling, the researchers proved that melanoma tumour cells can actually do both at the same time.
“This discovery might have an impact on patient treatment,” said Professor Haass.
“There has been concern that using a drug to stops the tumour from growing might cause the cancer cells to switch and begin metastasizing. Once the initial drug activity wanes, tumour cells that have migrated may start to grow and generate metastatic disease.
“Now we know that this isn’t necessarily the case, however, this may differ from drug to drug.”
The finding was part of the laboratory’s work on understanding the biology of melanoma cells.
Melanoma tumours can contain numerous cells with not only different genetic mutations, but also dynamically different behaviour, according to Professor Haass.
“Most people think of a melanoma tumour as a big chunk of cells that are all the same, but this isn’t the case. Within tumours, there are different clusters of melanoma cells sitting next to each other.
“Each cluster can respond very differently to the drugs used to treat melanoma. A drug might kill one cluster, while another one continues to grow or even grow faster as the competition with the other cluster is gone.
“If we can identify these different clusters in a patient, we can help clinicians determine the best combination and timing of drugs to treat the melanoma.”
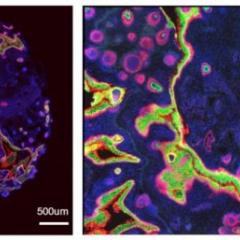
The team is using real-time imaging of melanoma cells in 3D culture and in vivo, to investigate the role of these subpopulations. With this method, they can colour code the different behaviour of the cells and watch them moving around the in the tumour.
They are the only group in Australia and one of the few groups internationally who are using this sophisticated technology.
It has enabled them to identify potential new markers for drug therapies and potential new targets to use in simultaneously targeting differential subpopulations.
Professor Haass is also looking at how melanoma cells interact with the surrounding microenvironment—that is the extracellular matrix, blood vessels, immune and blood cells. He believes we could harness this microenvironment to stop melanoma cells from growing and invading other parts of the body.
“One of my postgraduate students has a cool study that shows the melanoma cells can get stopped by the microenvironment under certain conditions. They can’t squeeze through,” said Professor Haass.
“We are looking at this phenomenon to see if we can manipulate melanoma tumours to prevent their growth and spread.”
In addition to these studies, Professor Haass and an industry partner are investigating a possible way to enhance melanoma immunotherapy, using patients’ blood samples before and after treatment.
In Australia, melanoma is the third most commonly diagnosed cancer, accounting for more than 13,000 cases in 2016 and more than 1700 deaths.[1] If caught early, the cancer is usually curable. In many cases, however, the cancer has advanced and begun metastasizing or spreading to other parts of the body before diagnosis. By this point, the cancer can be difficult to cure.
This article was originally published by The Translational Research Institute. For more information click here.